Freezing rain, snow showers, car covered with dirt and salt spray, gray skies, darkness before we are ready for it. It’s definitely November in Wisconsin. My daily trips to Spooner seem short by comparison but they still are challenged with this weather.
I am learning how different a nursing home is from a rehab hospital – something I knew in my head but experience emphasizes it. Some days I am dismayed with the care the husband is given. Some days I feel much better about it. Several days I have had to wake him up and get his care started without help. The weekend was actually frightening with the staff being stretched thin and several incidents happening. I wasn’t sure Dennis was getting his meds or his feedings on time or at all.

Today I arrived late in the morning and all was peaceful and calm, the room was straightened and my husband was dressed and sleeping in his recliner. But let me tell you about yesterday…
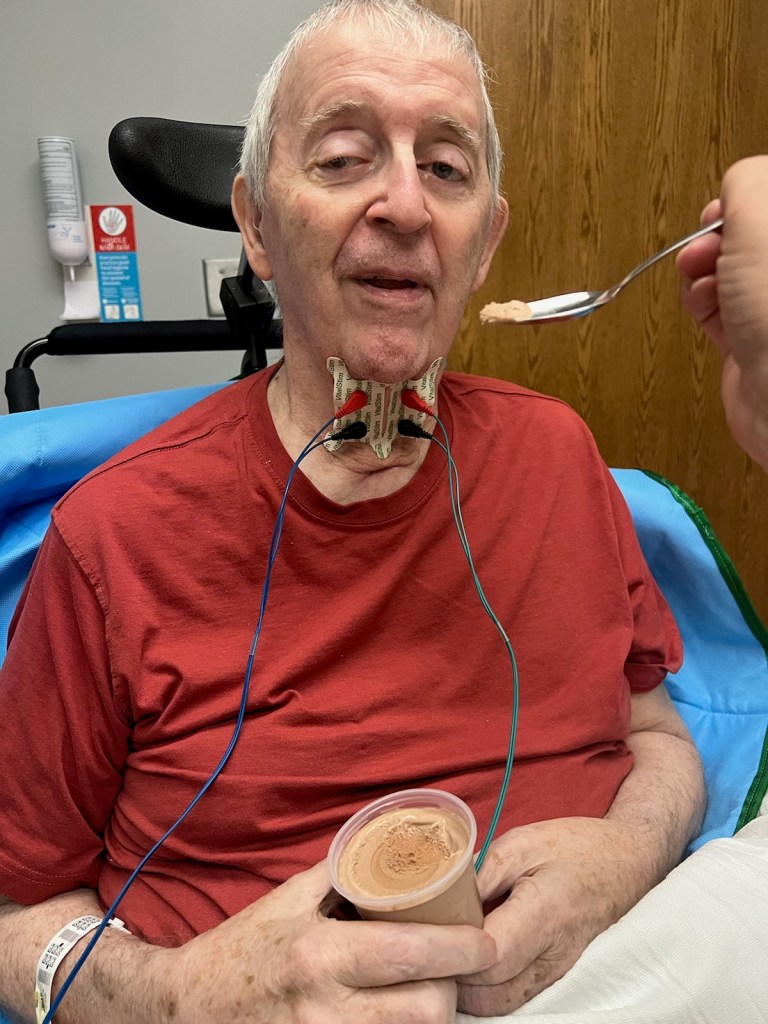
Somewhere between his speech therapy session, which I was told went well, and his PT session something happened to Dennis. He was much different, being unable to participate in his PT transfers, unable to keep himself upright, and not being responsive to questions and general talk. He stiffened and was hard to move and slept for hours without his usual requests for position change or the urinal. I wondered if he was having a second stroke. After a couple hours without improvement, it was decided to pack him up and go to the hospital ER for evaluation. The ambulance came and got him.
I will mention here that he didn’t want to go and had to be talked into it. He saw nothing wrong with the way he was feeling. I knew something wasn’t right but didn’t know what. I’m the one who has to think about him needing emergency care. Emergency care in the nursing home amounts to an LPN doing chest compressions while waiting for a phone request for a doctor to show up – no monitoring, medications or personnel familiar with running a code. I pretty much scared him into going by telling him to get evaluated or risk dying in his bed.
At the ER we got so much information over the next five hours. He had a urinary tract infection but the good news was that he didn’t have Covid, didn’t have pneumonia, didn’t have a second stroke or heart problems. He got a dose of antibiotic in his feeding tube and another ride back to Maple Ridge in the ambulance.
I went home and was settling down to sleep when the nursing home called to say Dennis was on the way back to the ER because his feeding tube had come out. I had heard a popping sound while watching the ER nurse give the antibiotic but I assumed she was familiar with the ports on his feeding tube. I asked her if one of them was the inflation port for the balloon that kept the tube in place in the stomach. She said yes, but didn’t seem concerned. The balloon had broken but the tube didn’t slip out until back at the nursing home when they moved him about.
Dennis got a new tube put in and two more rides in the ambulance. What a night. And, as I said, he is pretty hard to wake up again today, but with reason.
I find it hard to sit and watch him sleep. He is unable to wake up long enough to focus on anything or communicate more than a word at a time. I hope that as the urinary tract infection clears up, he will revive, be himself again and resume therapy.
Our setback matches perfectly with the gray, wet, coldness outside. It’s November.