It’s the first day of December, and in honor of the new month I want to move forward and record our next adventure. The last four months since the husband’s stroke, have been full of hospitals, rehab, and nursing home for him. For me, it’s been hours in the car traveling to keep an eye on his condition, his progress, his caregivers. I’ve spent very little time at home and didn’t feel like doing much when I was there.
So, that’s all changing tomorrow. I can’t believe tomorrow is nearly here, at last. We will be packing up and leaving the nursing home at 2 pm to travel the half hour to our home at Par Place. Some of our transfers took two hours from start to finish but for some reason this one has taken ten days. I have been pushing and being the “squeaky wheel” the whole time – ever since I became convinced that Dennis would be better off, and happier, at home. There have been obstacles in our path, and one after the other, they have melted away.
The new life, well, I debated whether to call it new or more specifically, different. The different life for me will be staying at home and being a full-time caregiver. Hopefully it will give Dennis some consistency and more attention.
However, there is the question of whether or not we can actually do this as well as we would like. I’ve put a lot of thought and effort into getting equipment, supplies, formula for his tube feedings, and helpers. Most weekdays I will have help for two hours in the morning and two hours in the evening. I have friends who will come and give me breaks for exercise, and appointments around town. B
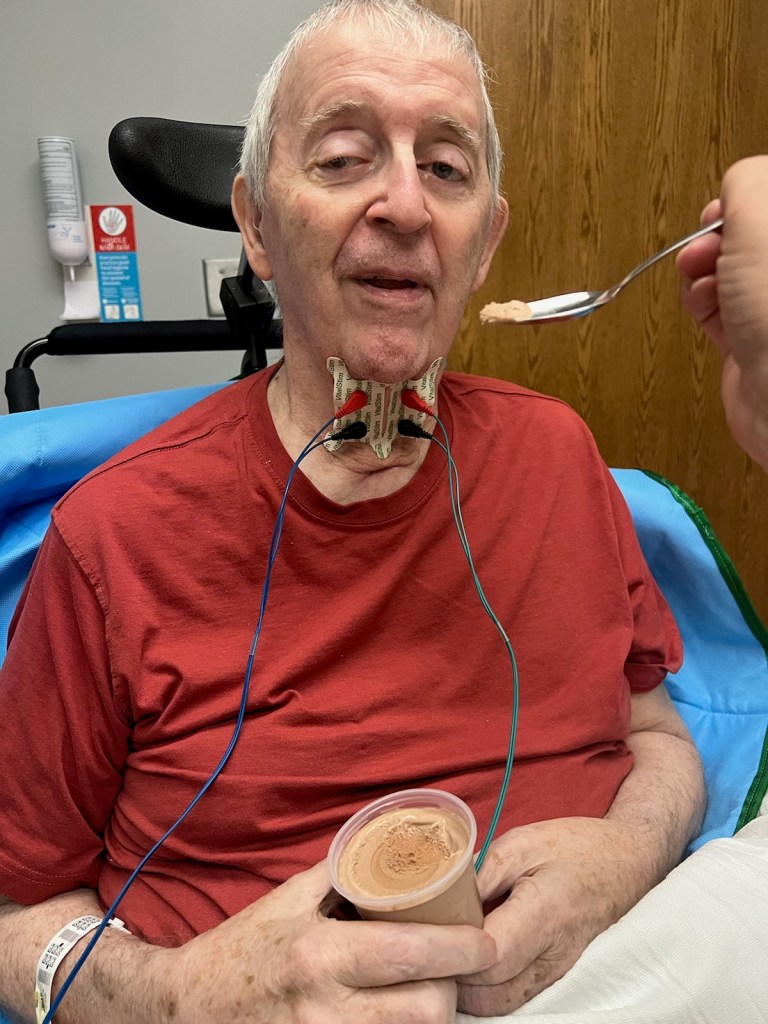
ut he is quite helpless, weak, and often disoriented. All his meds and nourishment have to go through the stomach tube (PEG tube). He is bowel and bladder incontinent. He will have to be moved with a Hoyer lift from his bed to his recliner or wheelchair. He sleeps most of the time. Fortunately, he is still himself on those occasions when he wakes up and talks. He knows me and his friends. He remembers that he is coming home on Friday.
So, because this may be the last thing he and I do together, I want to remember how it went, what we said to each other, and how it felt to know that life might very well be coming to a close. We have talked some about these things, but only recently has he at last confessed that he couldn’t think well enough to be in charge of his own health care. “I trust my wife”, he told the Hospice nurse.
Although we had the conversation, and an evaluation, we won’t be getting help from Hospice. They won’t accept him as long as he has a feeding tube, sorry but those are the rules. I was upset for about five minutes and then remembered that God had been asked to lead and direct, and he is faithful. I was then relieved that Dennis wouldn’t have to be affected by their rules. One less decision that I would have to make.
Every day in December, to write and remember, that is my goal. So, more tomorrow. I’m sure it will be an exciting day…